DENTAL CAVITATIONS - Do I HAVE THEM???
Dental Cavitations: Who Should Look, How to Evaluate, and How to Support Healing
By Tamara Lyday, DO — TLC: The Lyday Center
Published: January 15, 2026
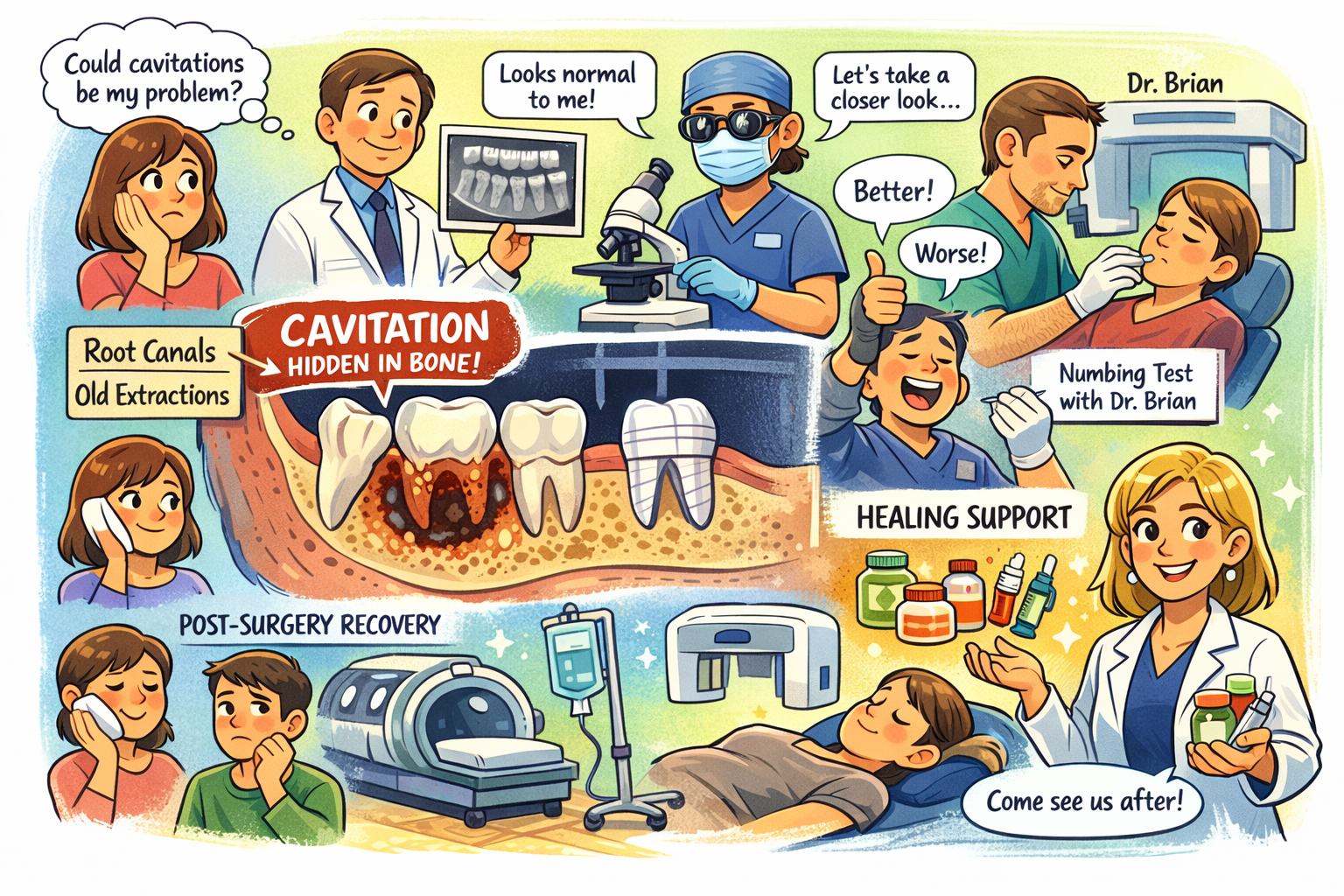
Quick take: If you have lingering symptoms with a dental history (root canals, extractions, wisdom teeth removal), a hidden dental focus can be part of the picture. Imaging can help—but even advanced scans may miss problems. Proper evaluation requires a team and sometimes an exploratory surgical approach. If cavitation surgery is appropriate, whole‑person prep and recovery can make a meaningful difference.
What are “dental cavitations”?
“Cavitation” is a commonly used term for areas of poorly healed bone after a tooth extraction or other dental procedure—sometimes called neuralgia‑inducing cavitational osteonecrosis (NICO), fatty degenerative osteonecrotic jawbone (FDOJ), or chronic osteitis. Not all clinicians agree on definitions or prevalence, but many patients with complex, chronic symptoms report improvement after a properly identified and treated focus of infection is addressed.
Possible clues include stubborn facial or jaw pain, sinus pressure, ear symptoms, headaches, trigeminal neuralgia‑like flares, unexplained fatigue, inflammatory or neurological symptoms that resist standard care—and a dental history that fits (see below).
Note: This article is for education; it doesn’t diagnose or treat. Please partner with qualified dental and medical professionals.
Who should consider cavitations as part of their story?
You might explore this if you have persistent symptoms plus one or more of the following histories:
Root canals (especially long‑standing or symptomatic teeth)
Tooth extractions, including sites that felt “slow to heal”
Wisdom teeth removal
Dental trauma, implants, or repeated procedures in the same area
Chronic sinus or ear complaints without a clear cause
Chronic inflammatory conditions (e.g., mold‑illness/CIRS, Lyme‑associated illness) with ongoing flares despite doing “all the right things”
This does not mean cavitations are your cause—but they may deserve thoughtful evaluation in the right context.
How are cavitations evaluated?
1) Clinical history and exam
A skilled biological/holistic dentist will map symptoms, dental history, and anatomical clues.
2) Imaging: helpful, but not definitive
Standard dental X‑rays often do not detect cavitations reliably.
Cone‑beam CT (CBCT) can be very helpful in experienced hands, but even with good imaging and interpretation, lesions can be missed or look non‑specific.
3) Diagnostic local anesthetic blocks (what I’ve seen in practice)
Some clinicians, such as Dr. Brian at Howard Dental, use procaine injections at suspected sites. The idea: if symptoms improve when the area is numbed, the site might be a contributor. This can be a useful clue, but it isn’t perfect:
Many people’s symptoms are nebulous or fluctuating.
Some patients (like me!) may actually feel worse after injections—even when a focus exists—so a “worse with procaine” response does not necessarily rule it out.
4) The uncomfortable truth
Even with great imaging and a skilled dentist, the only definitive way to identify some cavitations is surgical exploration (“going digging”) with appropriate debridement and pathologic evaluation. That decision should be made carefully with your dental surgeon after weighing risks/benefits.
What to expect if a cavitation is treated
When a true focus of infection/necrotic bone is removed and the area heals properly, the immune system can finally process burdens it couldn’t “see” before. Patients sometimes notice changes in systemic symptoms, energy, or inflammation over the following weeks to months. Outcomes vary—some feel better quickly; others need broader support as the body recalibrates.
Preparing your body (and mind) for possible surgery
At TLC, we favor whole‑person preparation tailored to your case. Examples may include:
Environment & basics: good air (HEPA in bedroom), hydration, protein‑forward meals, steady electrolytes
Gentle movement & breathwork to support circulation and lymph
Nervous system support: brief daily practices that downshift stress (you’ll heal better)
Adjuncts (as appropriate): hyperbaric oxygen (HBOT), IV nutrient therapy, photobiomodulation/LED, peptides where indicated, and lymph‑moving bodywork
Personal note: I recently enjoyed a craniosacral treatment after work to help move lymph—layered in with my own HBOT, IV support, movement, peptides, and more. Healing loves coherence.
Post‑operative care: Set yourself up for a smoother recovery
Work with your dental surgeon and medical team. Common elements include:
Wound care and infection prevention exactly as directed
Pain control that’s effective and gut‑friendly
Protein + micronutrients for tissue repair; hydration + electrolytes
Sleep, light movement, and lymph support (e.g., gentle walks, head/neck drainage techniques approved by your team)
Consider supportive modalities (HBOT, IVs, red/near‑infrared light) when appropriate to your case
Important: Every protocol is individualized. This article does not provide medical or dental advice. Always follow your surgeon’s instructions.
When to not chase cavitations
If symptoms are mild, improving, or you have unaddressed basics (ongoing mold exposure, micronutrient deficits, untreated sleep apnea, etc.), it may be premature to pursue jaw surgery. Foundations first; escalations later.
How to get evaluated
Start with a consult at TLC for a whole‑person review and care plan.
If appropriate, we’ll help coordinate with experienced biological dentists for imaging, exam, and (when indicated) diagnostic blocks.
We’ll outline pre‑hab and aftercare so you’re not navigating blind.
Ready to explore? Contact us to schedule: [phone] • [email] • [website]
FAQ
Will regular X‑rays show cavitations?
Often no. Even CBCT can miss them; clinical judgment matters.
Are anesthetic “test injections” definitive?
No—they’re a clue, not a proof. Relief suggests involvement; worsening or no change doesn’t rule it out.
Is surgery always the answer?
No. We consider the whole picture first and proceed only if benefits outweigh risks.
How long until I feel different after surgery?
Varies. Some notice shifts within days; others over months—especially with systemic issues.
A TLC update
We’re cheering on Jasmine as she steps away from TLC to focus on her nursing studies. We’re grateful for her care and wish her the very best on her educational journey.
The bottom line
Cavitations are not the hidden cause for everyone—but for the right person with the right history, investigating jawbone healing can be a missing piece. If you’re considering this path, don’t go it alone. Come see us—we’ll help you prepare, partner, and recover with a plan that respects your body’s wisdom.
This content is for educational purposes only and is not a substitute for individualized medical or dental advice.